Definition
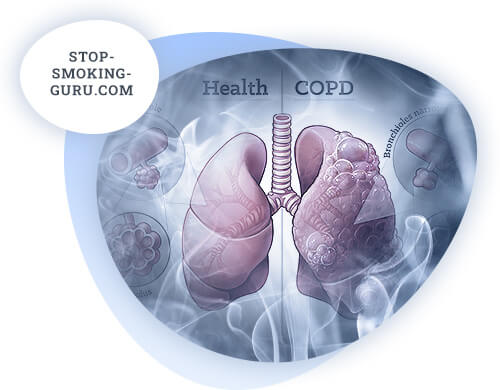
Over the last 15-20 years there has been a significant increase in the incidence of chronic obstructive pulmonary disease (COPD) worldwide. In September 2000 at the next congress of European Respiratory Society there was announced a draft document named GOLD (Global Initiatie for chronic Obstructive Lung Disease) - the result of WHO experts work on COPD problem, repeatedly revised during the next years. It defines COPD as "...a disease characterized by partially irreversible airflow limitation. Airflow limitation is usually of a steadily progressive nature and is caused by an abnormal inflammatory response of lung tissue to irritation by various pathogenic particles and gases" (GOLD-2006). According to GOLD-2007 the main diagnostic criteria of COPD are clinical (cough, sputum production, dyspnea), anamnestic (presence of risk factors) and functional (postbronchodilatation SPEF1 less than 80% of proper in combination with SPEF1/EL ratio less than 70%). The term "COPD" currently includes chronic obstructive bronchitis, chronic purulent obstructive bronchitis, pulmonary emphysema (secondary, arising as a morphological change in the lungs as a result of long-term bronchial obstruction), pneumosclerosis, pulmonary hypertension, chronic pulmonary heart. Each of these concepts reflects peculiarities of morphological and functional changes at different stages of COPD. The disease is an urgent problem, since the consequences of the disease are limitation of physical performance and disability of patients.
Epidemiology
In Russia, according to the results of calculations using epidemiological markers, it is supposedly about 11 million patients, while according to official medical statistics - about 1 million. This discrepancy is due to the fact that the disease is diagnosed in late stages, when the treatment cannot slow down the steadily progressing pathological process. This explains the high mortality rate of COPD patients. According to the European Respiratory Society, only 25% of cases are diagnosed in time. In recent years, there has been a worldwide upward trend in the incidence of the disease: from 1990 to 1997 it increased by 25% in males and 69% in females.
Etiology
The European Respiratory Society offers the following classification of risk factors according to their significance:
- Probability of Factor Significance. External factors. Internal factors. Smoking. Occupational hazards (cadmium, silicon). Deficiency of α1-antitrypsin. Environmental air pollution (SO2, NO2, O3). Occupational hazards. Low socio-economic status. Passive smoking during childhood. Prematurity. High levels of IgE. Bronchial hyperreactivity. Familial nature of the disease. Possible adenovirus infection. Vitamin C deficiency. Genetic predisposition (blood group A(II), lack of IgA).
Smoking
Smoking is the main risk factor (80-90% of cases). The mortality rate from COPD among smokers is the highest; they develop airway obstruction and dyspnea more quickly. However, cases of COPD occurrence and progression have also been reported in non-smokers. Dyspnea appears at approximately 40 years of age in smokers and 13-15 years later in non-smokers. According to WHO statistics the Russian Federation ranks fourth in the world by the number of cigarettes smoked (after China, the USA and Japan). The prevalence of tobacco smoking among Russian residents is fairly high and has been rising over the past 15 years.
The Smoking Index (MSI) is the main indicator used to calculate the frequency of tobacco smoking. It is calculated as follows: number of cigarettes smoked per day x number of months a year that the person smoked (usually 12). There are data, including domestic medicine, that allow using this indicator to estimate the likelihood of developing COPD.
- MSI > 120 - smoking leads to chronic obstructive bronchitis.
- MSI > 160 - smoking poses a risk for COPD.
- MSI > 240 - smoking inevitably leads to the development of COPD.
The MSI also depends indirectly on length of smoking, with an area of guaranteed harm being the MSI between 60 and 720.
Occupational factors
The most harmful occupational factors are dusts containing cadmium and silicon. The mining industry is the leading cause of COPD. Occupations with increased risk: miners, construction workers, workers in contact with cement, workers in metallurgy (due to melted metal vapors) and pulp and paper industry, railroad workers, workers in grain and cotton processing. In Russia, among coal miners there are a large number of people with lung diseases of dust etiology, including dusty bronchitis. Smoking increases the adverse effects of dust.
Hereditary predisposition
The role of heredity is supported by the fact that not all long-term smokers become COPD patients. The most studied genetic risk factor is a rare inherited deficiency of α1-antitrypsin (A1AT), which inhibits serine proteinases in the systemic bloodstream. In the United States, congenital A1AT deficiency has been detected in less than 1% of patients with CNSL.
Pathogenesis
The following processes play the greatest role in the pathogenesis of COPD:
- inflammatory process,
- Proteinase and antiproteinase imbalances in the lungs,
- oxidative stress.
Chronic inflammation affects all parts of the airways, lung parenchyma and vessels. Over time, the inflammatory process destroys the lungs and leads to irreversible pathological changes. Enzyme imbalances and oxidative stress can result from inflammation, environmental or genetic factors.
In the pathogenesis of COPD, impaired functioning of the local lung defense system is important. This system is represented by nonspecific and specific mechanisms. The action of nonspecific defense mechanisms, in particular phagocytosis, is directed against any foreign agent, while specific mechanisms are realized through the factors of local immune response. There are several links of local pulmonary defense system:
- mucociliary apparatus - ciliated cells and rheological properties of mucus;
- humoral link - immunoglobulins, lysozyme, lactoferrin, antiproteases, complement, interferon;
- cellular link - alveolar macrophages (AM), neutrophils and lymphocytes, as well as bronchoassociated lymphoid tissue (BALT).
The leading link in the development of the disease is a violation of the escalatory function of the mucociliary apparatus, which is the main protective mechanism of the respiratory tract. It is known that effectiveness of bronchial clearance depends on rheological properties of bronchial secretion, coordinated work of ciliary apparatus, contraction of smooth muscles of bronchial walls.
Prolonged smoking impairs escalatory function of mucociliary apparatus.
Hypersecretion of mucus (one of the earliest signs of COPD) occurs under the influence of tobacco smoke and various pollutants. This hypersecretion is combined with changes in rheological properties of bronchial secretion, which becomes more viscous and dense due to an increase in sialo-, sulfo- and fucomucin. Viscous sputum, tobacco smoke, pollutants, viral and bacterial toxins suppress cilia function and at the same time lead to impaired ciliated cell function due to reabsorption of excess mucin from the bronchial lumen.
A change in the viscoelastic properties of bronchial secretion is accompanied by significant qualitative changes in its composition: the content in the secretion of nonspecific components of local immunity, possessing antiviral and antimicrobial activity - interferon, lactoferrin and lysozyme - decreases. Along with this, the content of secretory IgA decreases. All this leads to violation of mucociliary transport, development of mucociliary failure, accumulation of mucus in the lumen of bronchi and its subsequent infection with microbial flora.
Disorders of mucociliary clearance and the presence of local immunodeficiency create optimal conditions for colonization of microorganisms. Thick and viscous bronchial mucus with reduced bactericidal potential is a good breeding ground for various microorganisms (viruses, bacteria, fungi). Under certain conditions, these patients have an activation of respiratory infection. This may be a consequence of reactivation of autoflora or the result of superinfection with pneumotropic microorganisms, to which COPD patients are highly sensitive.
Parallel to mucociliary transport disorder in the bronchi, so-called "oxidative stress" is formed (combination of increased oxidant activity and decreased antioxidant activity), which contributes to neutrophil activation during inflammation. Activated neutrophils are the main source of free oxygen radicals (superoxide, hydrogen peroxide, hypochlorous acid) in the airways; in addition, they have increased activity of myeloperoxidase, neutrophil elastase of circulating blood, which concentrate in the lungs in large amounts under the influence of trigger factors (tobacco smoke causes neutrophils migration to the terminal airway). In COPD there is an increase in the number of neutrophils, macrophages and T-lymphocytes, mainly CD8+.
Neutrophils. Sputum, bronchoalveolar lavage show increased number of activated neutrophils. Their role in COPD is not yet clear. Smokers without COPD also show sputum neutrophilia. Examination of induced sputum shows elevated concentrations of myeloperoxidase and human neutrophil lipocaine, indicating neutrophil activation. The number of neutrophils in bronchoalveolar lavage also increases with exacerbation. Neutrophils secrete proteinases: neutrophil elastase, neutrophil cathepsin G and neutrophil proteinase-3.
Macrophages are found in large and small bronchi, lung parenchyma, as well as in places of destruction of alveolar wall during emphysema development, which is revealed by histological examination of sputum and lavage, bronchial biopsy and investigation of induced sputum. Macrophages secrete tumor necrosis factor α (TNF-α), interleukin 8 (IL-8), and leukotriene-B4 (LTB4), which promotes neutrophil chemotaxis. CD8+ cells detected in bronchial biopsies secrete perforin, granzyme-B, and TNF-α; these agents cause cytolysis and apoptosis of alveolar epitheliocytes.
Eosinophils. Levels of eosinophilic cationic peptide and eosinophilic peroxidase are elevated in induced sputum of COPD patients. This indicates the possibility of their presence. This may not be related to eosinophilia - increased neutrophil elastase activity may account for the degranulation of eosinophils when their numbers are normal.
Epithelial cells. Exposure to air pollutants such as nitrogen dioxide (NO2), ozone (O3), diesel exhaust on nasal and bronchial epithelial cells leads to the synthesis and release of inflammatory mediators (eicosanoids, cytokines, [adhesion molecules], etc.). Epitheliocyte regulation of E-selectin adhesion molecules functioning, responsible for neutrophil involvement in the process, is disturbed. At the same time, the secretion of bronchial epithelial cell cultures obtained from COPD patients in the experiment produces lower amounts of inflammatory mediators, (TNF-α or IL-8), than similar cultures from nonsmokers or smokers but without COPD.
Inflammatory mediators
Tumor necrosis factor α (TNF-α), interleukin 8 (IL-8), and leukotriene-B4 (LTB4) play the greatest role in COPD. They are capable of destroying lung structure and supporting neutrophilic inflammation. The damage they induce further stimulates inflammation by releasing chemotactic peptides from the intercellular matrix.
LTB4 is a powerful neutrophil chemotactic factor. Its content in the sputum of COPD patients is elevated. Production of LTB4 is attributed to alveolar macrophages.
IL-8 is involved in selective involvement of neutrophils and is probably synthesized by macrophages, neutrophils and epithelial cells. It is present in high concentrations in induced sputum and lavage in COPD patients.
TNF-α activates nuclear factor-B transcription factor (NF-B), which in turn activates the IL-8 gene of epitheliocytes and macrophages. TNF-α is detected in high concentrations in sputum as well as in bronchial biopsy specimens from COPD patients. In patients with severe weight loss, serum TNF-α levels are elevated, suggesting that the factor may be involved in the development of cachexia.
Other agents are also involved in inflammation in COPD. Some of them are presented below:
- Mediator. Abbreviated Function. Study Material. In which group the content in the study material is elevated. Control group. Macrophage chemotactic protein-1MCP-1. Monocyte recruitment, macrophage recruitment. Bronchoalveol. lavage. COPD patients, smokers. Non-smokers, former smokers. Macrophage inflammatory protein-1βMIP-1β. Involvement of monocytes, T lymphocytes. Bronchoalveol. lavage. COPD patients. Non-smokers, smokers, former smokers. Macrophage inflammatory protein-1αMIP-1α. Involvement of monocytes, T lymphocytes. Expression in epitheliocytes. COPD patients. Smokers. Granulocyte-macrophage colony stimulating factorGM-CSF. Stimulates activity of neutrophils, eosinophils, monocytes, and macrophages. Bronchoalve lavage. COPD patients, content increases during exacerbations. Transforming growth factor-βTGF-β. Inhibits natural killer activity, reduces proliferation of B- and T-lymphocytes. Expression in epitheliocytes, eosinophils, and fibroblasts. COPD patients. Endothelin-1ET-1. Vasoconstriction. Induced sputum. COPD patients.
Pathophysiological changes in COPD include the following pathological changes:
- mucus hypersecretion,
- cilia dysfunction,
- lung hyperinflation,
- parenchymal destruction and pulmonary emphysema,
- gas exchange disorders,
- pulmonary hypertension,
- pulmonary heart disease.
Bronchial obstruction in patients with COPD is formed by reversible and irreversible components. The irreversible component is formed as a result of smooth muscle spasm, edema of bronchial mucosa and mucus hypersecretion, resulting from the release of a wide range of anti-inflammatory mediators (IL-8, tumor necrosis factor, neutrophil proteases and free radicals). Irreversible component of bronchial obstruction is determined by developing emphysema, epithelium hyperplasia, smooth muscle cell hypertrophy and peribronchial fibrosis. Due to the disturbance of elastic properties of the lungs, respiratory mechanics changes and expiratory collapse is formed, which is the most important cause of irreversible bronchial obstruction. Peribronchial fibrosis is a consequence of chronic inflammation; it influences the formation of irreversible component less than emphysema. Development of emphysema leads to reduction of the vascular network in the areas of lung tissue incapable of gas exchange. As a result, blood flow is redistributed in the remaining parts of the pulmonary tissue, there are pronounced ventilation and perfusion disorders. Irregular ventilation-perfusion relationships are one of the important elements of COPD pathogenesis. Perfusion of poorly ventilated areas leads to decreased arterial oxygenation, excessive ventilation of underperfused areas leads to increased dead space ventilation and delayed C02 release. Chronic hypoxia leads to compensatory erythrocytosis - secondary polycythemia with corresponding increase in blood viscosity and microcirculation disorders, which aggravate ventilation-perfusion mismatch. An important component of COPD pathogenesis is respiratory muscle fatigue, which in turn reduces respiratory function and aggravates ventilation disorders. Thus, arterial hypoxia develops due to uneven ventilation and impaired ventilation-perfusion relations. The outcome of COPD is development of precapillary pulmonary hypertension due to vasoconstriction of small pulmonary arterioles and alveolar vessels as a result of alveolar hypoxia. Right ventricular hypertrophy gradually develops. Chronic pulmonary heart syndrome is formed; in decompensation it first manifests as transient and then persistent right ventricular failure.
Pathomorphology
The basis is an inflammatory process affecting all structures of the lung tissue: bronchi, bronchioles, alveoli, pulmonary vessels.
Morphological changes are characterized by epithelial metaplasia, death of epithelial cilia, hypertrophy of submucosal glands secreting mucus, proliferation of smooth muscles in the airway wall. All this leads to mucus hypersecretion, occurrence of sputum, violation of bronchial drainage function. Narrowing of the bronchi as a result of fibrosis occurs. Lung parenchyma damage is characterized by the development of centrilobular emphysema, alveolar-capillary membrane changes and disorders of diffusion capacity, leading to the development of hypoxemia.
Respiratory muscle dysfunction and alveolar hypoventilation lead to chronic hypercapnia, vasospasm, pulmonary arterial remodeling with thickening of the vascular wall and decreased vascular lumen. Pulmonary hypertension and vascular damage lead to the formation of pulmonary heart. Progressive morphological changes in the lungs and associated respiratory dysfunctions lead to the development of cough, hypersecretion of sputum, and respiratory failure.
Clinical picture
Cough is the earliest symptom of the disease. It is often underestimated by patients, being expected with smoking and exposure to pollutants. At the first stages of the disease it appears episodically, but later it occurs daily, occasionally appearing only at night. Outside the exacerbation, the cough is usually not accompanied by sputum. Sometimes there is no cough in the presence of spirometric evidence of bronchial obstruction.
Sputum is a relatively early symptom of the disease. In the initial stages, it is secreted in small amounts, usually in the morning, and has a mucous character. Purulent, profuse sputum is a sign of exacerbation of the disease.
Dyspnea appears about 10 years later than coughing, and is first noted only during significant and intense physical exertion, intensifying with respiratory infections. Dyspnea is more often of the mixed type, and expiratory dyspnea is less common. In later stages, dyspnea ranges from shortness of breath during normal exercise to severe respiratory failure, and becomes more pronounced over time. It is a frequent reason for seeking medical attention.
The Medical Research Council (MRC) Dyspnea Scale is a modification of the Fletcher Scale to assess the severity of dyspnea:
- Degree. Severity. Description. No. Dyspnea only with very intense exertion. Light. Dyspnea during fast walking, slight lifting. Medium. Shortness of breath makes you walk slower than people of the same age. Severe. Shortness of breath makes you stop when walking about every 100 meters. Very severe. Dyspnea makes it impossible to go outside the house or appears when changing clothes.
Clinical forms. Examination of COPD in the far advanced stage of the disease reveals 2 types of clinical picture: emphysematous and bronchitic.
Clinical variants of COPD:
- Sign. Bronchitic type. Emphysematous type. Correlation of cough and dyspnea. Cough prevails. Dyspnea prevails. Bronchial obstruction is pronounced. Less pronounced. Hyperventilation of the lungs is weakly expressed. Strongly expressed. Cyanosis diffuse blue-gray. Pulmonary heart at an early age. In old age. Polycythemia is often very rare. Cachexia not characteristic often. Fatal outcome in young years. In old age.
Emphysematous form of COPD is mainly associated with panacinar emphysema. Such patients are figuratively called "pink puffers", because to overcome prematurely occurring expiratory collapse of the bronchi they exhale through folded lips and are accompanied by a peculiar puffing. Dyspnea at rest prevails in the clinical picture due to decreased lung surface area for gas diffusion. Such patients are usually thin, their cough is more often dry or with a small amount of thick and viscous sputum. The complexion is pink, because sufficient oxygenation of blood is maintained by maximum possible increase in ventilation. The limit of ventilation is reached already at rest, and patients are very poorly tolerated by physical exertion. Pulmonary hypertension is moderately pronounced, since the reduction of the arterial channel caused by atrophy of interalveolar septa does not reach significant values. Thus, emphysematous type of COPD is characterized by predominant development of respiratory failure.

In bronchial form of COPD there is constant hypersecretion, which causes increase of resistance on inhalation and on exhalation, which contributes to significant impairment of ventilation. In turn, a sharp decrease in ventilation leads to a significant decrease in alveolar content, subsequent disturbance of perfusion-diffusion relations and blood shunting. This causes characteristic blue tint of diffuse cyanosis in patients of this category. Such patients are obese, the clinical picture is dominated by cough with profuse sputum secretion. Diffuse pneumosclerosis and obliteration of blood vessel lumen, significant hypoxemia, erythrocytosis, persistent pulmonary hypertension lead to rapid development of pulmonary heart and its decompensation. More often the given types are combined in one and the same patient, but it is often possible to note predominance of emphysematous or bronchitic component.
Disease phase
COPD exacerbation is a worsening of well-being for at least two consecutive days, occurring acutely. The aggravation is characterized by increased cough, an increase in the amount and composition of sputum, and increased shortness of breath. During an exacerbation, therapy is modified and other medications are added. Below are the criteria of some working groups:
Criteria for exacerbation of COPD:
- Anthonisen et al. criteria, 1987. BTS (British Thoracic Society) criteria, 1997. Working Group criteria, 2000. Major Criteria. Increased dyspnea. Increased amount of sputum. Increased "pusiness" of sputum. Small criteria. Infection of the upper respiratory tract. Fever. Whistling breathing. Increased cough. Increase in heart rate or HR by 20% or more. Increased amount of sputum. Increased "festering" of sputum. Increased dyspnea. Wheezing. Congestion in the chest. Fluid retention. Respiratory signs. Increased dyspnea. Increased amount and "pusiness" of sputum. Increased cough. Frequent shallow breathing. Systemic signs. Increased body temperature. Increased heart rate. Disturbance of consciousness.
Exacerbation is diagnosed on the basis of a set of criteria. Anthonisen et al. also distinguish 3 types of COPD exacerbations:
- Type I exacerbation - a combination of all three major criteria;
- Type II exacerbation - presence of two of the three big criteria;
- Type III exacerbation - a combination of one major criterion and one or more minor criteria.
Complications of COPD:
- acute or chronic respiratory failure;
- secondary polycythemia;
- chronic pulmonary heart failure;
- congestive heart failure;
- pneumonia;
- spontaneous pneumothorax;
- pneumomediastinum.
Formulating the diagnosis
According to the international GOLD program (2003), patients with COPD should indicate the phase and severity of the disease, the course of the disease, the patient's condition (exacerbation or remission), and then list the complications that occurred during the course of the disease.
Example formulation of the diagnosis:
- COPD, predominantly bronchitic type, stage IV, extremely severe course, exacerbation, chronic purulent bronchitis, exacerbation. Chronic decompensated pulmonary heart, H III, DN III.
Classification
Stratification of severity (stage)
Stratification is based on two criteria: clinical, which includes cough, sputum production, and dyspnea, and functional, which considers the degree of irreversibility of airway obstruction. They also previously distinguished risk of COPD as stage 0 disease, but recent GOLD texts have abandoned this category because there is insufficient evidence that patients who have "risk of disease development" (chronic cough, sputum production with normal measures of external respiratory function) necessarily develop stage I COPD. The reported OEF1 values are post-bronchodilator values, that is, the severity is assessed by bronchial patency values after bronchodilator inhalation:
Stage I. Mild
- SPH1/FEL less than 70 % of proper
- SPE1 more than 80 % of proper
- Presence or absence of chronic symptoms (cough, phlegm)
SPH1 remains within the statistical average, while the ratio of SPH1 to ELF becomes lower than 70% of the proper value. This index reflects early manifestation of bronchial obstruction detected by spirometry. It characterizes the change of exhalation structure, i.e. during the 1st second of forced exhalation the patient exhales the index of the average statistical norm, however in relation to the ELF this percentage decreases to 70% of the norm, that reveals an individual violation of the function of external respiration.
Stage II. Average
- SPH1/EPHEL less than 70 % of proper
- SPH1 is less than 80% of proper
- Presence or absence of chronic symptoms (cough, phlegm, dyspnea)
This stage, in which patients seek medical care for dyspnea or exacerbation of the disease, is characterized by an increase in obstructive impairment (SPH1 is 50-80% of the proper values). There is increase of symptoms of disease and dyspnea, appearing at physical load.
Stage III. Severe
- SPH1/EPHEL is less than 70% of the proper value
- SPE1 is less than 50 % of proper
- Presence or absence of chronic symptoms (cough, phlegm, dyspnea)
It is characterized by further increase in airflow limitation (SPR1 is 30-50% of the proper values), increase in dyspnea, and frequent exacerbations.
Stage IV. Extremely severe
- SPH1/EPHEL is less than 70 % of the proper value
- SPH1 is less than 30% of its proper value, or less than 50%, combined with chronic respiratory insufficiency.
At this stage, quality of life deteriorates markedly, and exacerbations may be life-threatening. The disease acquires a disabling course. It is characterized by extremely severe bronchial obstruction (BEF1 < 30% of the proper values or < 50% in the presence of respiratory insufficiency).
COPD occurs and progresses long before the appearance of significant functional abnormalities determined by instrumentation. During this time, inflammation in the bronchi leads to severe irreversible morphological changes, so this stratification does not address the issue of early diagnosis and timing of treatment initiation.
Diagnosis
Diagnosis of COPD is based on anamnestic findings, clinical manifestations, and the results of pulmonary ventilation function tests. The disease usually develops in middle age and progresses slowly. Risk factors include smoking habits, occupational hazards, atmospheric pollution, smoke from home heating appliances, kitchen smells, and chemical irritants. The main clinical manifestations are cough with sputum and shortness of breath. Coughing and sputum production may occur only in the morning hours. The cough usually occurs throughout the day, rarely only at night. The amount of sputum is usually small, outside exacerbations it is mucous, often sputum is discharged after a prolonged cough. Dyspnea usually progresses with time. It increases with physical exertion, in humid weather, and with exacerbations. When examining the patient, scattered dry rales of different timbre are heard. Sometimes auscultatory phenomena in the lungs are not detected, and to identify them it is necessary to offer the patient to make forced exhalation. In advanced stages of COPD there are clinical signs of pulmonary emphysema (enlarged anteroposterior dimension of the chest, widened intercostal spaces, boxy sound on percussion). At development of chronic respiratory failure and pulmonary hypertension "warm" acrocyanosis, swollen cervical veins are noted. The golden diagnostic standard is detection of partially irreversible bronchial obstruction by studying the ventilatory function of the lungs. The volume of forced expiratory volume in the first second (FEF1) is reduced and decreases with disease progression. To assess the reversibility of obstructive ventilation disorders, a pharmacological test is performed. The initial value of SPR1 is compared with the same parameter 30-45 min after inhalation of sympathomimetic (400 mcg) or cholinolytic (80 mcg), or combination of bronchodilators with different mechanisms of action. An increase in BEP by more than 15-12% or by 200 ml or more indicates the reversibility of bronchial obstruction. In bronchial asthma, high air volume increases are common, while in COPD they are minimal. This test is included in the criteria for differential diagnosis of COPD.
Treatment and prevention
The goals of COPD treatment are as follows:
- Prevention of worsening of the course of the disease,
- Improvement of tolerance to physical activity,
- Prevention and treatment of complications,
- Prevention and treatment of exacerbations,
- reduction of mortality.
Preventive measures
Smoking cessation
It is established that smoking cessation allows to slow the increase of bronchial obstruction. Therefore, treatment of tobacco addiction is relevant for all patients suffering from COPD. In this case conversations of medical personnel (individual and group) and pharmacotherapy are the most effective. There are three programs of tobacco addiction treatment: short (1-3 months), long (6-12 months) and program of smoking intensity reduction.
Prescribing medications is recommended for patients with whom the physician's conversations have proven ineffective. Their use should be considered in people who smoke less than 10 cigarettes a day, adolescents, and pregnant women. Unstable angina, untreated peptic duodenal ulcer, recent acute myocardial infarction and cerebrovascular disease are contraindications to nicotine replacement therapy.
Increase of patients' awareness allows to increase their ability to work, improve their state of health, forms the ability to cope with the disease, increases the effectiveness of treatment of exacerbations. Forms of patient education vary from distribution of printed materials to seminars and conferences. The most effective is interactive training, which is held in a small workshop.
Control of occupational factors
Combating occupational hazards that lead to the development of respiratory tract injuries consists of two groups of measures:
- Providing individual protection for the respiratory organs;
- reducing the concentration of harmful substances in the air of the working area through various technological measures.
Each of these methods prevents the ingress of harmful substances into the human body, thus reducing the risk of developing COPD.
COPD treatment
COPD treatment programs are determined by the stage of the disease, severity of symptoms, severity of bronchial obstruction, frequency and severity of exacerbations, presence of respiratory failure and other complications, concomitant diseases. In all stages of COPD, special attention is paid to the exclusion of risk factors, patient education, preventive and rehabilitative measures.
The basic principles of managing patients with a stable course of COPD are as follows:
- The volume of treatment increases as the severity of the disease increases. Its reduction in COPD, in contrast to bronchial asthma, is usually impossible.
- Drug therapy is used to prevent complications and reduce the severity of symptoms, the frequency and severity of exacerbations, improve exercise tolerance and quality of life of patients.
- It should be borne in mind that none of the available medications does not affect the rate of bronchial permeability decrease, which is a distinctive feature of COPD.
- Bronchodilators are central in treatment of COPD. They reduce the severity of the reversible component of bronchial obstruction. These agents are used on demand or regularly.
- Inhaled glucocorticoids are indicated in severe and extremely severe COPD (with a forced expiratory volume in 1 s (FEF1) less than 50% of proper and frequent exacerbations, usually more than three in the last three years or one or two in one year, for which oral steroids and antibiotics are used.
- Combination therapy with inhaled glucocorticoids and long-acting β2-adrenomimetics has a significant additional effect on lung function and clinical symptoms of COPD compared with monotherapy with each drug. The greatest effect on the frequency of exacerbations and quality of life is observed in COPD patients with SPH1<50% of proper. These drugs are preferably prescribed in an inhaled form containing their fixed combinations (salmeterol/fluticasone propionate, formoterol/budesonide).
- Prolonged use of tablet glucocorticoids is not recommended due to the risk of systemic side effects.
- At all stages of COPD, physical training programs that increase exercise tolerance and reduce the severity of dyspnea and fatigue are highly effective.
- Long-term oxygen administration (more than 15 hours a day) to patients with respiratory insufficiency increases survival.
Bronchodilators
These include β2-adrenomimetics, cholinolytics, and theophylline. The principles of bronchodilator therapy for COPD are as follows.
- The preferred route of administration of bronchodilators is inhalation.
- Change of pulmonary function after short-term prescription of bronchodilators is not an indicator of their long-term efficacy. A relatively small increase in SPR1 can be combined with significant changes in pulmonary volumes, including a decrease in residual lung volume, which contributes to a reduction in the severity of dyspnea in patients.
- The choice between β2-adrenomimetics, cholinolytics, theophylline depends on their availability, individual sensitivity of patients to their action and the absence of side effects. In elderly patients with concomitant cardiovascular diseases (CHD, heart rhythm disorders, arterial hypertension, etc.), cholinolytics are preferred as first-line drugs.
- Xanthines are effective for COPD, but due to the possibility of side effects, they are second-line drugs. When prescribing them, it is recommended to measure theophylline concentration in blood. It should be emphasized that only long-acting theophylline (but not eufylline and theophedrine!) have a positive effect on the course of COPD.
- Long-acting inhaled bronchodilators are more convenient, but also cost more than short-acting agents.
- Regular treatment with long-acting bronchodilators (tiotropium bromide, salmeterol and formoterol) is indicated for moderate, severe and extremely severe COPD.
- A combination of several bronchodilators (e.g., cholinolytics and β2-adrenomimetics, cholinolytics and theophylline, β2-adrenomimetics and theophylline) may improve efficacy and reduce the possibility of side effects compared with monotherapy with one drug.
COPD inhalation therapy (D.Tashkin, CHEST, 2004)
COPD stage. Inhaled therapy. Short-acting bronchodilators as needed (ipratropium, fenoterol, salbutamol and/or combinations thereof). Tiotropium + fenoterol or salbutamol as needed. Salmeterol or formoterol + ipratropium, fenoterol, or a combination thereof. Tiotropium + salmeterol or formoterol + low-dose methylxanthines (if not effective enough). Salmeterol or formoterol (if effect insufficient + tiotropium and/or salbutamol or fenoterol, and/or low-dose methylxanthines). Tiotropium + salmeterol or formoterol + inhaled steroids (salbutamol or fenoterol as needed).
Cholinolytics have traditionally been considered the basic bronchodilators for the treatment of COPD. M-cholinolytics block muscarinic receptors in the smooth muscles of the tracheobronchial tree and suppress reflex bronchoconstriction, as well as prevent acetylcholine-mediated stimulation of sensitive vagus nerve fibers when exposed to various factors, thereby providing bronchodilator and preventive effects. Ipratropium bromide and tiotropium bromide (prolonged preparation) of this group are widely used. Ipratropium bromide is a quaternary isopropyl derivative of atropine. After a single application of 40 micrograms (2 inhalations) of ipratropium bromide, the action begins after 20-40 minutes, reaches a maximum after 60 minutes and lasts for 5-6 hours. The drug in doses with bronchodilator effect does not penetrate into CNS, inhibits salivary gland secretion to a lesser extent, has no effect on motor activity of tracheal epithelium and does not change BP and HR. Tiotropium bromide binds to M1-, M3- and, to a lesser extent, to M2 cholinoreceptor species: half-life of binding to M1- and M3-receptors is 14.6 and 34.7 hours respectively, for M2-receptors - only 3.6 hours. Accordingly, the duration of binding of tiotropium bromide with cholinoreceptors allows using it once a day. Having low systemic absorption from the respiratory tract (elimination half-life does not exceed 1 h) it practically does not cause atropine-like side effects.
b2-agonists have a rapid effect on bronchial obstruction, improving the well-being of patients in the short term. With prolonged use of b2-agonists resistance to them develops, after a break in medication their bronchodilator effect is restored. Decrease of b2-adrenoceptors efficiency and, as a consequence, worsening of bronchial patency are related to desensitization of b2-adrenoreceptors and decrease of their density due to long-term exposure to agonists, as well as to development of "ricochet syndrome", characterized by sharp bronchospasm. "Ricochet syndrome" is caused by blockade of bronchial b2-adrenoreceptors by metabolic products and impaired drainage function of the bronchial tree due to the development of "lung closure" syndrome. Contraindications to the use of b2-agonists in COPD are hypersensitivity to any component of the drug, tachyarrhythmias, cardiac defects, aortic stenosis, hypertrophic cardiomyopathy, decompensated diabetes mellitus, thyrotoxicosis, glaucoma, threatened abortion. This group of drugs should be used especially cautiously in elderly patients with concomitant cardiac pathology.
Features of b2-agonists of short (salbutamol, fenoterol) and long (formoterol, salmeterol) action.
b2-Agonist. Dosage. Pharmacodynamics. Side effects. Salbutamol. Dose inhaler 100 mcg/inhalation dose 100-200 mcg/6-8 h (maximum 800-1200 mcg per day). Dischaler 200-400 mcg/blister 200-400 mcg/6-8 h (maximum 1600 mcg/day. Nebulizer 2.5-5.0 mg every 6 hr. Onset of action: 5-10 min. Maximal action: 30-90 min. Duration of effect: 3-6 h. Most common side effects: Tremor. Headache. Agitation. Hypotension. Hot flashes. Hypokalemia. Tachycardia. Dizziness. Fenoterol. Dosed inhaler 100 mcg/inhaled dose 100-200 mcg/6-8 h (maximum 800-1200 mcg per day). Nebulizer 0.5-1.25 mg every 6 hr. Onset of action: 5-10 min. Maximal action: 30-90 min. Duration of effect: 3-6 h. Monitoring of side effects. Analysis of symptoms. BP control. HR control. Electrolyte control. Formoterol 12 mcg/capsule 12 mcg/12 h (maximum 48 mcg/day). Onset of action: 10-20 min. Duration of effect: 12 h. Salmeterol. Dosed inhaler 25 µg/inhalation dose 25-50 µg/12 h (maximum 100 µg/24 h). Dischaler 50 mcg/blister 50 mcg/12 hr. Discus 50 mcg/inhalational dose 50 mcg/12 hr. Onset of action: 10-2 min. Duration of effect: 12 h.
Methylxanthines are added to therapy when the first two groups of drugs are not effective enough; they reduce systemic pulmonary hypertension and enhance respiratory muscle function.
Glucocorticoids. These drugs have pronounced anti-inflammatory activity, although in patients with COPD it is expressed significantly less than in patients with asthma. Short (10-14 days) courses of systemic steroids are used to treat exacerbations of COPD. Prolonged use of these drugs is not recommended because of the risk of side effects (myopathy, osteoporosis, etc.).
They have been shown to have no effect on the progressive reduction of bronchial patency in COPD patients. Their high doses (e.g., fluticasone propionate 1000 mcg/day) can improve patients' quality of life and reduce the frequency of exacerbations of severe and extremely severe COPD.
The reasons for the relative steroid resistance of airway inflammation in COPD are the subject of intense research. It may be due to the fact that corticosteroids increase the life span of neutrophils by inhibition of their apoptosis. The molecular mechanisms underlying glucocorticoid resistance are poorly understood. There are reports that smoking and free radicals reduce the activity of histone deacetylase, a target of steroids, which may reduce the inhibitory effect of glucocorticoids on the transcription of "inflammatory" genes and weaken their anti-inflammatory effect.
Recently, new data have been obtained on the effectiveness of combined agents (fluticasone propionate/salmeterol 500/50 mcg, 1 inhalation twice a day and budesonide/formoterol 160/4.5 mcg, 2 inhalations twice a day, budesonide/salbutamol 100/200 mgk 2 inhalations twice a day) in COPD patients with severe and extremely severe course. Their long-term (12 months) prescription has been shown to improve bronchial patency, reduce the severity of symptoms, the need for bronchodilators, the frequency of moderate to severe exacerbations, and improve patients' quality of life compared with monotherapy with inhaled glucocorticoids, long-acting β2-adrenomimetics and placebo.
Mucolytics (mucoregulators, mucokinetics) are indicated for a very limited number of patients with stable COPD and are used in the presence of viscous sputum; they do not significantly affect the course of the disease. Long-term use of mucolytics (N-acetylcysteine, ambroxol) is promising for prevention of COPD exacerbation.
Vaccines. Influenza vaccination reduces the severity of exacerbations and mortality in COPD patients by about 50%. Vaccines containing killed or inactivated live influenza viruses are usually administered once in October through the first half of November.
There is insufficient data on the effectiveness of the pneumococcal vaccine, which contains 23 virulent serotypes of this microorganism, in COPD patients. However, some experts recommend its use in this disease to prevent pneumonia.
If dyspnea intensifies, the amount of sputum increases and its purulent nature is prescribed antibacterial therapy. The main etiologically significant microorganisms of infectious exacerbations of COPD are Streptococcus (Str.) pneumoniae, Haemophilus (H.) influenzae, Moraxella (M.) catarrhalis. Based on the clinical situation in exacerbations of COPD a tentative determination of the microbial spectrum is possible. In mild exacerbations the most common clinically relevant microorganisms are H.influenzae (untypable and unencapsulated forms), S.pneumoniae, M.catarrhalis. In more severe exacerbations and the presence of unfavorable prognostic factors (marked bronchial obstruction, respiratory failure, decompensation of concomitant pathology, etc.), often requiring hospitalization in intensive care units, the proportion of the above microorganisms is reduced, while the proportion of H.influenzae producing - lactamases increases; Gram-negative bacteria, in particular various members of the Epteobacterium family.
Antibacterials used to treat exacerbations of COPD
Antibacterial agent. Spectrum of action. Advantages. Disadvantages. Beta-lactams: Ampicillin. Amoxicillin. Co-amoxiclav. Gram-positive and gram-negative flora. The drugs are commonly known, toxic effects are rare, and oral forms are affordable. Do not inhibit mycoplasma and chlamydia. Resistant strains are possible. Sensitization to beta-lactams is common. Macrolides: Azithromycin. Clarithromycin. Midecamycin. Roxithromycin. Spiramycin. Erythromycin. Gram-positive flora, mycoplasma, chlamydia. The drugs are generally known, toxic and allergic reactions are rare, high tissue concentrations are created in the lungs, long-lasting postantibiotic effect. They are ineffective against Haemophilus influenzae and Moraxella (azithromycin and clarithromycin are more active). Resistant strains are possible. Fluoroquinolones: Ofloxacin. Ciprofloxacin. Fluoroquinolones of the 3rd-4th generation: Levofloxacin. Moxifloxacin. Gram-positive and gram-negative flora, mycoplasma, chlamydia. Optimal spectrum of action, high tissue concentrations in lungs, allergic reactions are rare, used once a day. Toxic reactions are rare, the cost is higher than that of the generic fluoroquinolones of previous lines. Tetracyclines: Doxycycline. Gram-positive and gram-negative flora, mycoplasma, chlamydia. Optimal spectrum of action. The drug is generally known toxic and allergic reactions are rare. It is affordable. Resistant strains of Gram-positive and Gram-negative flora are frequent.
Oxygen therapy
Respiratory failure is known to be the main cause of death in COPD patients. Correction of hypoxemia with oxygen supply is a pathogenetically sound method of treatment. There are short-term and long-term oxygen therapy. The first one is used in acute exacerbations of COPD. The second is used in extremely severe course of COPD (with SPH1<30% of the proper one) constantly or situationally (at physical load and during sleep). The aim of oxygen therapy is to increase partial oxygen tension (RaO2) in arterial blood to not less than 60 mm Hg, or saturation (SaO2) to not less than 90% at rest, during exercise and sleep.
With a stable course of COPD, continuous long-term oxygen therapy is preferable. It is proved to increase survival rate of COPD patients, reduce the severity of dyspnea, progression of pulmonary hypertension, reduce secondary erythrocytosis, the frequency of episodes of hypoxemia during sleep, improve exercise tolerance, quality of life and neuropsychiatric status of patients.
Indications for long-term oxygen therapy in patients with COPD of extremely severe course (with OEF1 < 30% of proper or less than 1.5 L):
- RaO2 less than 55% of proper, SaO2 less than 88% in the presence or absence of hypercapnia;
- RaO2 55-60% of proper, SaO2 89% in the presence of pulmonary hypertension, peripheral edema associated with decompensated pulmonary heart or polycythemia (hematocrit over 55%).
Prolonged oxygen treatment should be administered for at least 15 h per day. Gas flow rate is usually 1-2 l/min, if necessary, it can be increased up to 4 l/min. Oxygen therapy should never be administered to patients who continue to smoke or suffer from alcoholism.
Compressed gas cylinders, oxygen concentrators and cylinders with liquid oxygen are used as oxygen sources. Oxygen concentrators are the most economical and convenient for home use.
Oxygen is delivered to the patient with the help of masks, nasal cannulas, transtracheal catheters. The most convenient and widely used are nasal cannulas, which allow the patient to receive oxygen-air mixture with 30-40% O2. It should be noted that oxygen therapy is one of the most expensive methods of COPD patients treatment. Its introduction into everyday clinical practice is one of the most urgent medical and social problems in Russia.
Rehabilitation measures
Rehabilitation is a multidisciplinary program of individual care for COPD patients designed to improve their physical, social adaptation and autonomy. Its components are physical training, patient education, psychotherapy, and rational nutrition.
In our country, it traditionally includes sanatorium treatment. Pulmonary rehabilitation should be prescribed for COPD of moderate severity, severe and extremely severe course.
It has been shown to improve performance, quality of life and survival of patients, to reduce shortness of breath, frequency of hospitalizations and their duration, to suppress anxiety and depression. The effect of rehabilitation persists after its completion. Sessions with patients in small (6-8 persons) groups with the participation of specialists of various profiles over the course of 6-8 weeks are optimal.
In recent years much attention has been paid to rational nutrition, as loss of body weight (>10% within 6 months or > 5% during the last month) and especially loss of muscle mass in COPD patients is associated with high mortality. Such patients should be advised a high-protein, high-calorie diet and metered exercise with an anabolic effect.
Prognosis
The prognosis for recovery is unfavorable. The disease is characterized by a steadily progressive course, leading to the development of early disability and reduced life expectancy. Complications of COPD are acute or chronic respiratory failure, secondary polycythemia, chronic pulmonary heart failure, congestive heart failure, pneumonia, spontaneous pneumothorax, pneumomediastinum. To assess the prognosis, the following parameters play a decisive role: possibility of elimination of provoking factors, patient's adherence to treatment, socio-economic conditions. Unfavorable prognostic signs are severe comorbidities in COPD, development of cardiac and respiratory insufficiency, elderly age of patients.
By: Dr. Alan David